Introduction
Immunoglobulin light chain (AL) amyloidosis is a rare disease caused by a clonal plasma cell dyscrasia producing monoclonal light chains that misfold and form amyloid fibrils which can deposit in a variety of tissues and organs. This deposition of amyloid fibrils can lead to progressive organ impairment, multi-organ failure, and death if left untreated. High-dose melphalan and autologous stem cell transplantation (HDM/SCT) is known to improve patient outcomes with hematologic complete responses (CR) rates of 25-67%.
Hematologic CR is currently defined as the absence of monoclonal protein in serum and urine by immunofixation electrophoreses and normal serum free light chain ratio (FLCR). Studies have shown that even among patients achieving a normal FLCR after initial therapy with HDM, persistent elevation of the involved FLC (hiFLC) predicts poor prognosis. Serum half-life of FLCs is approximately 2-6 hours, even with diminished glomerular filtration rates, and could be a tool for early treatment response evaluation. We sought to determine the extent to which early FLC responses after HDM/SCT predict hematologic complete response (CR) at 6 months.
Methods
We analyzed patients with AL amyloidosis who underwent HDM/SCT from 2012-2019 at Boston Medical Center. Exclusion criteria included death within 100 days, lack of FLC data at any time point, pre-SCT normal FLC concentrations and ratio, and chronic renal insufficiency (serum creatinine >1.3 mg/dL) with a normal FLC ratio. All subjects received a total of 140-200 mg/m2 melphalan IV in equally divided doses on days -3 and -2. Stem cells were infused on day 0. FLC measurements were obtained early in the peri-SCT period (< 1 month), at 6 months, and at 12 months after HDM/SCT. The patients were evaluated for response according to the consensus response criteria at 6 months. Statistical analysis to compare CR at 6 months and early post-SCT free light chain levels was performed by Chi-square with significance considered at p<0.05.
Results
Of the 113 patients with AL amyloidosis treated with HDM/SCT during the specified time period, 32 were excluded (4 died within 100 days of SCT, 15 had normal FLCs pre-SCT, 5 lacked data, and 8 had chronic renal insufficiency (Cr >1.3 mg/dL) with normal FLCR. A total of 81 subjects (females=30) were analyzed. Median follow-up from SCT was 27.6 months (range, 6-145). Median time of early post-SCT FLC measurement was 8 days (range, 7-30).
Median age at diagnosis was 58 years (range 30-79) and the iFLC was lambda in 81.5% (n = 66) of patients. Median number of bone marrow plasma cells was 10% (range, 1-50). The mean absolute involved FLC was 196 mg/L ±221 prior to SCT, 60 mg/L ± 77 in the early post-SCT period, 92 mg/L ± 152 at 6 months post-SCT. In early post-SCT period, 39.5% (n=32) had iFLC <20 mg/L, 28% (n=16/57) had dFLC<10 mg/L, and 84% (n=48/57) had normal FLCR.
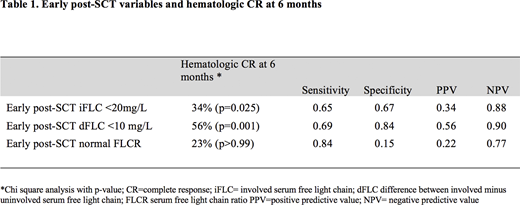
Early post-SCT dFLC <10 mg/dL and early post-SCT iFLC <20 mg/L were statistically associated with prediction of hematologic CR at 6 months (p=0.025 and p=0.001, respectively). However, early post-SCT normal FLCR was not associated with predicting hematologic CR at 6 months. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of early post-SCT iFLC <20 mg/L, dFLC <10 mg/L and normal FLCR to predict hematologic CR at 6 months are presented in table 1.
Conclusion
This study concludes that achievement of dFLC <10 mg/L and iFLC <20 mg/L in the early post-SCT period is associated with prediction of hematologic CR at 6 months. Early post-SCT dFLC <10 mg/L could be considered a tool for early evaluation of treatment response following HDM/SCT in AL amyloidosis.
Key words: immunoglobulin light chains; AL amyloidosis, HDM/SCT
Sarosiek:Spectrum: Research Funding. Sanchorawala:Caelum: Research Funding; Prothena: Research Funding; Celgene: Research Funding; Takeda: Research Funding; Proclara: Other: advisory board; Abbvie: Other: advisory board; UpToDate: Patents & Royalties; Oncopeptide: Research Funding; Regeneron: Other: advisory board; Caleum: Other: advisory board; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal